Macular Surgery
What is the Macula?
The macula is the central area of the retina where fine-detail vision for reading, recognizing faces, and driving is located. The retina is the light sensitive inner lining in the back of the eye that is like the film in a camera. Anatomically, the macula is located in the straight ahead position of the eye and is at the center of the retina. If the retina were a target, the macula would be the bull’s eye. Although the macula is a small portion of the total retina, it is the most important area for the precise visual tasks required of modern life.

What are the common anatomical problems of the macula?
Problems of the macula can be explained by an abnormal interaction be- tween the retina and the natural gel in the back of the eye called the vitreous. The vitreous gel is a clear substance that fills the majority of the back of your eye. Sometimes, abnormal attachments of the vitreous to the retina or surface contraction of the retina can lead to various problems including macular hole, macular pucker, and vitreomacular traction.
Macular Holes
The initial symptoms of macular holes include blurring of vision and distortion. As the hole opens further, a blind spot can develop resulting in difficulty with vision. This occurs due to abnormal tangential traction on the macula. The traction in macular hole is likened to pulling on the edges of a button hole. As the fabric is pulled apart, the hole gapes open. By removing the pulling forces on the macula, we allow the tissue to come back together, eliminating the gape, thereby closing the hole. Patients with a macular hole in one eye have a 14% chance of developing a macular hole in their other eye.
Observation of small and recent macular holes is often recommended, since occasionally they will resolve spontaneously. For older, larger and progressively enlarging macular holes, surgery is required to restore vision and prevent further visual loss. Surgical and visual success is best if the eye is operated on within the first 3 months of onset.
To repair the hole, your surgeon will perform vitrectomy surgery and remove a fine layer of the retina known as the internal limiting membrane. Removal of this tissue has been associated with a higher rate of hole closure and a lessened risk of hole re-opening. With this technique, there is about a 95% chance of successful hole closure with a single surgery.
At the end of the surgery, your surgeon will place a gas bubble in the eye. At this point, proper head positioning helps to ensure successful healing. You will be asked to maintain a face-down position for the first week. This position places the gas bubble over the hole to help prevent reopening. Your body will absorb this gas bubble over the course of about 3-6 weeks. As long as the gas bubble is in the eye, you should avoid laying flat on your back. The vision will be blurred, and you will be restricted from flying, traveling to high altitude, and scuba diving as this can lead to the dangerous elevation of eye pressure from expansion of the bubble.
Successful closure of the hole has been reported without face down positioning. The success rate is slightly less than with face-down positioning, yet still quite good. At Retina Associates of Florida, we believe in tailoring surgery to the needs of our patients. If you are interested in undergoing macular hole surgery without face-down position, let your surgeon know so we can discuss whether you would be a favorable candidate. With recurrent or especially difficult macular holes, silicone oil may be substituted for intraocular gas or a blood patch made from the patient’s own plasma may be useful.

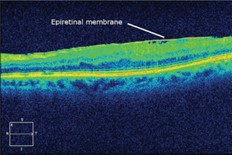

Epiretinal Membrane/Macular Pucker
Much like with macular holes, following separation of the vitreous gel the surface of the macula can contract and lead to wrinkling of the tissue known as macular pucker, epiretinal membrane, and cellophane maculopathy. One way to explain this is to imagine a piece of shrink wrap being heated. As it is heated, it contracts and wrinkles. Sometimes, a fine tissue can develop on the surface of the macula causing the macular tissues to wrinkle and swell. When this occurs, patients can notice blurred vision and frequently distortion or a change in image size compared to their non-affected eye. Macular pucker is relatively common occurring in about 6-10% of the population and does not always affect vision. The majority of patients will remain stable without any further changes in vision, but inflammation after ocular surgery has been associated with progression. Testing with a special grid known as an Amsler grid to monitor for progression is recommended.
Surgical removal involves vitrectomy and removal of the fine scar tissue causing the wrinkling. This procedure usually improves distortion and difference in image size, but, mild symptoms may persist. It is important to discuss with your surgeon the symptoms and level of difficulty that you are experiencing to decide whether surgery is right for you.
Macular Traction
As we age, it is normal for the collagen fibers in the vitreous gel inside the eye to slowly break down and liquefy. Occasionally, the vitreous remains strongly attached to the macula despite separation in other areas. As the rest of the vitreous pulls away, it can pull the macula upward creating blur and distorted vision. Occasionally, the strand of vitreous can come loose and the problem resolves. However, over a long period of time, a macular hole can develop, epiretinal membrane may form, or permanent vision loss can occur. You and your surgeon will determine whether your symptoms are significant enough to warrant surgery. An in-office procedure with positioning called “the dipping-bird technique” can relieve this condition in at least 50% of patients.
We place a gas bubble in the office and the patient will dip their head 10 times per hour for 3 days to try to mechanically free the adhesion. If this does not resolve the situation or if the patient is unable to position, surgical correction of the macular traction may be accomplished with vitrectomy surgery, which has a greater than 95% success rate. Once the taut band (“clothesline”) is cut, the macular tissue can settle back to its normal position and shape. Even when the traction is relieved, it can take several months for the contour and vision to improve.
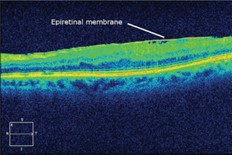
How are these macular problems evaluated?
Special imaging called ocular coherence tomography or OCT helps to con- firm the diagnosis in most cases. OCT is essentially a special photograph that allows us to look at the different layers of your macula in high magnification and fine detail. The OCT image can often show the precise anatomic abnormalities in the macula. Occasionally, an additional test called fluorescein angiography or FA can provide important additional information and help to exclude other causes of macular disease. The combination of your exam, OCT images, and possible FA pictures help guide our approach to your surgery.
What is micro-incisional/sutureless vitrectomy surgery?
Vitrectomy is the surgical removal of the naturally occurring vitreous gel in the back of the eye. It is usually performed under local anesthesia. Three small ports are inserted through the white part of the eye known as the sclera. A small cutter is placed through these ports to chop and suction the vitreous out of the back of the eye. A microscope is used to view the surgery along with a lighted probe to illuminate the inside of the eye. A continuous flow of saline solution is used to keep the eye inflated. Newer technologies allow us to perform these surgeries without stitches. The advantages of sutureless surgery include: Improved patient comfort, quicker recovery, quicker surgical times, and less trauma to eye tissues.
Understanding your risks
While complications are infrequent, they include: pain, bleeding or infection in the eye, detachment of the retina requiring additional surgery, cataract formation, increased or decreased eye pressure, decreased vision or field of vision, total loss of vision or the eye, among others. It is important that you discuss and understand the risks and benefits with your surgeon before surgery.
What can I expect after vitrectomy surgery?
Usually patients are pleasantly surprised at how comfortable the eye feels after surgery. A slight ache or scratchiness is not uncommon and should not require any more pain relief than can be provided by acetaminophen (i.e.Tylenol) or ibuprofen (i.e. Advil). If after taking these medications you still experience significant discomfort, it is important to let your surgeon know.
After surgery, you will need to avoid bending, straining, eye rubbing, or lifting anything over 15 pounds for the first 2 weeks. High impact activity including jogging, boating, and horse- back riding should also be avoided during the first 2 weeks post-operative. However, light activity such as walking or cycling are acceptable. Specific head positioning may be necessary. Your surgeon will usually prescribe drops for you to apply to the surgical eye. You will be provided instructions on how to take the drops at each visit.
Visual recovery after vitrectomy surgery is not always immediate. While approximately 90% of visual recovery occurs within the first 3 months, gradual improvement out to 1 year is not uncommon. This delay is usually due to macular swelling which arises from leakage of clear fluid from the retinal blood vessels. In many cases, additional treatment of the macular swelling with drops or injections can further improve the vision.