Flashes & Floaters
Flashes & Floaters Introduction
One of the most common problems that patients have when they visit a ret- inal specialist is seeing flashes of light or floaters in one or both eyes. These phenomena are called photopsias and are visual perceptions caused by events occurring inside the eye or elsewhere in the visual system. In order to understand the nature of these complaints it is important to understand the anatomy of the eye and brain and the physiology of vision.
Anatomy and Physiology
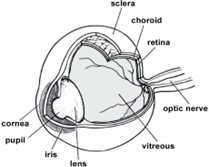
The eye is a spherical organ that allows us to see. In the front part of the eye is the cornea that lets light into the eye and the lens that focuses the light on the retina. The retina is in the back of the eye and acts like the film in an old camera or a CCD chip in a new digital camera or video camera. In the middle of the eye is a clear, gel-like substance called vitreous. In youth, the vitreous is a perfectly clear gel-like material with a consistency like Jell-O. With age, this gel liquefies and develops fluid cavities, condensations, and opacities (Figure 1).
In the middle of the eye is a clear, gel- like substance called Vitreous. In youth, the vitreous is aperfectly clear gel-like masterial with a consistency like jell-O. With age, this gel liquifies and developes fluid cavities, condensationsa, and opacities.
Vision is a complex physiologic process that begins when images are focused on the retina. The retina then converts these images into electrical impulses and transmits them along the optic nerve and optic radiations to the brain. An interesting part of visual physiology occurs at the optic chiasm where half of the visual information from the eye crosses over to the opposite side of the brain and half of the visual information stays on the same side. Because of this, the visual perceptions from the right side of the world are processed by the left brain and the images from the left side of the world are processed by the right brain. This is important in separating out visual phenomena that are caused by eye diseases that are uni- lateral and those that originate in the brain that appear to occur in both eyes.
Floaters
Floaters are visual perceptions of dark spots moving around in your vision. They are seen by all adults and are more prominent when there is bright light and a uniform background. Commonly, people see floaters best on a bright day against a clear blue sky or against a white wall. Another time when people see a lot of floaters is when they are swimming with goggles. (Figure 2). As we get older, the gel liquefies and the floaters become more prominent. If the vitreous separates or detaches from the back of the eye, then patients notice a sudden increase in floaters often accompanied by flashing lights off to the side. The flashing lights are usually of short duration like lightning strikes and are best seen in the dark. This will be covered in more detail in the section on vitreous detachment or vitreous separation.
There are some pathological conditions that can cause floaters as well. Eyes with diabetic retinopathy sometimes have bleeding in the eye and that causes floaters. Another common and benign cause of floaters is a condition called asteroid hyalosis. For reasons that aren’t exactly clear, white flecks of calcium- rich fats accumulate in the vitreous. If the eye has inflammation or uveitis, white cells and debris accumulate in the vitreous and cause prominent floaters. There are other unusual causes of floaters such as amyloidosis and lymphoma. Sometimes a biopsy of the vitreous has to be done to evaluate these more serious problems.
Flashing Lights
Flashing lights are usually caused by vitreous separation and subsequent traction on the peripheral retina or other causes of retinal traction. These flashing lights are peripheral, of short duration like a lightning strike, and occur in the dark. They are most commonly seen when people get out of bed in the middle of the night or early morning. They are less noticeable in daylight. Another cause of seeing lights is from a retinal detachment. In this case there is a glow or constant light in the periphery that either lasts for several minutes at a time or is present continually.
The other type of flashing light is from migraine phenomena. The patient usually sees a line of irregular flashing lights that are often described as “shards of glass” or like the fortifications on a medieval castle. They are often characterized as “shimmering.” Typically they gradually expand in diameter, and the episode may last up to 30 minutes. These flashing lights occur because of abnormal activity in the neural cells in the brain. Because of the anatomy of the visual system, they seem to occur in both eyes to either the right side or the left.
Vitreous Separation
The most common cause for the sudden onset of flashes and floaters is a vitreous detachment or vitreous separation. These two terms are used inter- changeably. As the vitreous ages it liquefies and develops fluid pockets and opaque material that cast shadows on the retina that causes floaters to appear in our vision. As this process of liquefaction progresses, it causes increased shear forces on the vitreo-retinal attachments and at one point in time, the vitreous will separate from the retina.
When that happens, patients usually see a shower of new floaters and when in the dark may see flashing lights in the periphery of their vision. When this happens, there may be tearing of retinal blood vessels or tearing of the retina. The tearing of the blood vessels can cause bleeding into the vitreous. This blood is seen as large, dark floaters. The vitreous separation may also tear the retina.
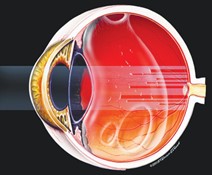
A torn retina allows the fluid from the vitreous cavity to pass through the hole and detach the retina (Figure 3). If the retina is detached, the corresponding field of vision is lost. There is usually no treatment necessary for a vitreous detachment unless there is also a tear in the retina. If the floaters are particularly bothersome, they can be removed surgically, but this is rarely indicated.
A few retinal doctors treat the floaters with a laser but this is not generally accepted therapy. If there is mild hemorrhage into the vitreous, the blood related floaters usually clear rather quickly and no treatment is necessary. If the hemorrhage is large and doesn’t clear spontaneously, then surgical intervention is sometimes necessary. The most significant problem associated with vitreous detachment is a tear in the retina. This is an emergency and needs to be treated right away to avoid progression to retinal detachment.

Migraine Phenomena, Aura and Headaches
Another common cause of flashing lights is the prodrome or aura of migraine. Migraine is a condition where brain cells exhibit abnormal activity and the patient experiences a curved line of flashing lights. While the flashing lights of a vitreous detachment are of short duration like a flash of lightning and are usually seen best in the dark, the flashing lights of a migraine are a curved line and take on a saw-tooth pattern or the pattern of medieval fortifications. They are persistent like a flashing neon sign or a police light. If the phenomenon is carefully observed, it will be apparent that the lights appear to be in both eyes to the right or left. They usually last about 15 to 30 minutes and are often accompanied by areas of blindness. Because of the anatomy of the visual system these flashing lights and areas of blindness appear to occur in both eyes in the same location.
Following the aura, some patients develop a severe, throbbing headache on the opposite side of where the flashing lights occur. Brain edema is thought to cause the headache of migraine that occurs following the aura. Some people get the headache without the aura and some people get the aura without the headache. In addition to the headache there can be light sensitivity and vomiting. Many people have very little problem with migraine and others find it severely debilitating. Migraine often occurs in clusters. You may have several headaches in a row and then be headache free for many months. If the headaches are severe and frequent, then medications exist to interrupt the migraine and to reduce their frequency and severity. Patients with severe problems need to see a neurologist. Migraines are hereditary and change over time. They are three times as common in women as in men. They often manifest during puberty, pregnancy, or menopause and can be related to the menstrual cycle. People who have migraine with aura have a higher incidence of stroke and the risk is increased in women who take estrogen for menopause or contraception.
Retinal Tears and Holes
Acute retinal tears almost always need prompt attention. The treatment for a retinal tear is to cause adhesion around the tear so that fluid cannot pass through the tear, under the retina, and cause a detachment. The retinopexy or treatment used to form the scar can be done with a laser or with a freezing technique called cryopexy.
For most eyes, laser is used to treat the tear. In patients with an anterior tear or in eyes with some peripheral cataract, cryopexy is the preferred treatment. Evaluations of both treatments have shown that there is no difference in success in preventing detachment. The treatment is 95% successful, but occasionally eyes do progress. The main risk of treatment is that it may not prevent the detachment. If the retina detaches, it indicates an active, sight-threatening process and a more involved procedure to treat the eye is necessary.
Retinal holes and tears without symptoms may or may not need to be treated. Treatment is usually recommended for tears where there is traction on the retina. Atrophic retinal holes are at a lower risk for detachment than retinal tears and depending upon the number of holes and other factors, observation may be the best choice. If an eye is about to have surgery, then it may be reasonable to treat holes and tears to prevent a detachment following the surgery.
Lattice Degeneration
Lattice degeneration is a common retinal abnormality that is present in seven percent of the population and is bilateral fifty percent of the time. It occurs in the periphery of the retina and does not affect vision but does lead to an increase in the risk of a patient developing retinal tears or retinal detachment. The general risk of developing a retinal detachment is 1 in 10,000. With lattice degeneration the risk increases to 0.3-0.5 percent, a fifty-fold increase in risk, but still small. In patients who have a detachment in one eye and lattice degeneration in the other eye the risk of detachment in the second eye is approximately 20 percent. Treatment to lattice degeneration is most often recommended for fellow eyes if there is a detachment in one eye. It is also done for some retinal holes, in patients with a strong family history of retinal detachment, and in eyes with extensive lattice degeneration. If someone is going to be away from medical care, as in a rural area or foreign country, then occasionally treatment is recommended.