Diabetic Retinopathy
Introduction
Diabetic retinopathy is a complication of diabetes that affects vision. Diabetic retinopathy is the leading cause of blindness in Americans under the age of 65, and currently the leading cause of new cases of legal blindness. The key to diabetic retinopathy is early detection by eye examinations, and control of blood glucose and blood pressure to reduce the risk of development and progression.
What is Diabetes?
Diabetes mellitus is a metabolic ab- normality that affects the way that the body uses sugar (known scientifically as glucose). There are two major categories of diabetes: juvenile onset diabetes or type I diabetes, and adult onset or type II diabetes. Patients with type I diabetes usually have the problem for many years before complications like diabetic retinopathy develop. Type II diabetes is much milder in onset and disturbances in sugar metabolism may be present many years before the diagnosis is made. Sometimes patients with adult-onset diabetes develop retinopathy before diabetes is discovered.
What causes diabetic complications?
The main complications of diabetes relate to the damage that the high blood sugar causes to the small blood vessels in the eye, the kidney, the peripheral nerves, the heart, the brain, and the blood vessels in the extremities. This damage to small vessels is called microangiopathy, and several scientific studies have shown this is directly related to the chronic elevation of blood sugar. In order to prevent or control these complications, the most important step is to control your blood sugar as best you can. In addition to blood sugar control, it is important to control other medical problems such as hypertension (high blood pressure) and hyperlipidemia (high fat in the blood). It is important that you discuss your disease in detail with your physician and come up with a plan to optimize the care of your diabetes.
How can I keep from going blind?
Several studies have provided over- whelming evidence that excellent diabetic control is the key to avoiding blindness and other complications of diabetes. It has been shown that chronically-elevated blood sugar directly damages the blood vessels leading to retinopathy, kidney disease, heart disease, strokes, and peripheral vascular disease. In the last few years, there have been major advances in diabetic management that include new oral medications, new forms of insulin, including pumps, and new technologies in glucose testing. Together with a physician skilled in diabetic care, these new advances should help all diabetics achieve better control and minimize the risk of blindness.
How do I know if I’m in good control?
The best test to evaluate diabetic control is the Glycated Hemoglobin test like a video camera and sends these signals to the brain along a “cable” called the optic nerve. Pressure in the eye is maintained by a system of fluid production and drainage. The drain- age area of the eye is at the edge of the iris and is called the trabecular meshwork. If this fluid flow is interrupted by blockage of the drain, the pressure in the eye becomes elevated and glaucoma develops.
Diabetes may affect the lens of the eye (cataract), the retina (diabetic retinopathy), the intraocular pressure of the eye (glaucoma) or the optic nerve (optic neuropathy). The conditions mentioned above occur in non-diabetic patients but are more common in patients with diabetes.
How does diabetes affect the eye and vision?
To understand how the eye is affected by diabetes, it is necessary to understand how the eye works and how we see the world around us. The eye works like a camera. The images from the world around us are focused by the cornea and lens on the retina, which is in the back of the eye and is similar to the film in a still camera or the CCD chip in a video camera. The light rays pass through the center of the eye where there is a clear, jelly-like substance called the vitreous. The retina processes the image like a video camera and sends these signals to the brain along a “cable” called the optic nerve. Pressure in the eye is maintained by a system of fluid production and drainage. The drainage area of the eye is at the edge of the iris and is called the trabecular meshwork. If this fluid flow is interrupted by blockage of the drain, the pressure in the eye becomes elevated and glaucoma develops.
Diabetes may affect the lens of the eye (cataract), the retina (diabetic retinopathy), the intraocular pressure of the eye (glaucoma) or the optic nerve (optic neuropathy). The conditions mentioned above occur in non-diabetic patients but are more common in patients with diabetes.

What is diabetic retinopathy?
The retina is a thin sheet of neural tissue at the back of the eye. Like most tissues in the body, there are blood vessels throughout the retina. These blood vessels are affected over time by elevated blood sugar. Diabetic retinopathy is classified as background retinopathy, (also known as non-proliferative retinopathy) and proliferative retinopathy. An important problem causing visual loss may occur in both types of retinopathy and is called macular edema. This occurs when the central area of the retina (the macula) swells and central vision decreases. This is the most common cause of visual loss in diabetes. The blood vessels may also close off, creating areas of the retina where there is no blood supply. These areas of the retina are said to be ischemic and appear as white, fluffy spots on the retina called cotton-wool spots.
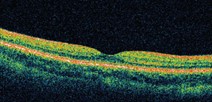
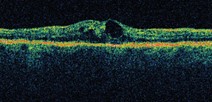
Office evaluation of diabetic retinopathy involves a careful eye exam including evaluation of the retina using a slit-lamp microscope and indirect ophthalmoscopy. Two additional tests are often used to evaluate the retina if vision-threatening retinopathy is present. A fluorescein angiogram is a test to evaluate whether the blood vessels in the retina are healthy. We do this by injecting an orange dye in your arm and taking pictures of your retina to see if there are any areas of poor circulation (ischemia) or to see if any dye leaks from the blood vessels. We have a new, unique technology to evaluate circulation in important areas that were previously not able to be evaluated (Optos Ultra-widefield angiography). A second important test is OCT (Optical Coherence Tomography). This test measures the thickness of the retina objectively, and it is particularly helpful in evaluating patients with edema and is also helpful in patients following treatment.
Classification of diabetic retinopathy:
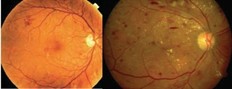
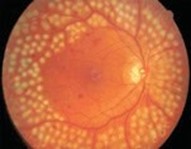
Mild background retinopathy Background retinopathy is classified as mild, moderate, or severe. Mild is the earliest sign of diabetic damage. Usually there are just a few microaneurysms, which are dilated blood vessels involving the capillaries of the retina. Often there are small hemorrhages in the retina as well. This mild retinopathy is a sign that blood vessel damage is occurring both in the retina and other susceptible body tissues. If your diabetic control is not good, this should be a wake-up call that improved control is necessary. This is not considered to immediately threaten vision. There is no specific ocular treatment for this stage other than careful observation and treatment of macular edema if it is present.
Moderate background retinopathy
Moderate diabetic retinopathy is a more advanced stage of background retinopathy. The microaneurysms and hemorrhages are more extensive and there are usually areas where the blood vessels have closed off that are called cotton-wool spots. They are often seen in patients who have associated high blood pressure. In some eyes there is leakage of plasma with yellow deposits called exudates. These areas of ischemia are signs of irreversible damage. If the areas of leakage are near the center of vision, they can cause visual loss by causing macular edema, which is explained in detail below. There is no specific ocular treatment for this stage unless there is macular edema, but again, control of blood sugar, blood pressure, and lipids is necessary to prevent more ocular damage and visual loss.
Severe or pre-proliferative diabetic retinopathy
Severe background retinopathy is a pre-proliferative stage that is the most advanced stage of non-proliferative retinopathy. In severe retinopathy, there are larger areas of ischemia, hemorrhages in all parts of the eye, the development of microvascular abnormalities, and dilation of retinal veins. Fifty percent of patients with this stage of retinopathy will go on and develop proliferative retinopathy within one year. Macular edema and exudates are common in advanced retinopathy. Fluorescein Angiogram showing microaneurysms and ischemia. Eye with moderate retinopathy showing hemorrhages, cotton-wool spots and exudates. Treatment of severe retinopathy usually entails laser photocoagulation to prevent progression to proliferative retinopathy and to prevent hemorrhage into the vitreous.
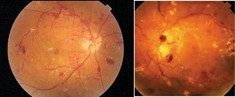
Early proliferative diabetic retinopathy
Proliferative retinopathy is the most advanced stage of retinopathy. In these eyes there are new blood vessels growing in the eye, hemorrhages into the vitreous, and retinal detachment caused by scar tissue. Fifty percent of patients in the diabetic retinopathy study were legally blind in five years unless there was treatment. The established and proven treatment for proliferative retinopathy is pan-retinal laser photocoagulation. It reduced the risk of blindness by fifty percent. Injection of anti-VEGF drugs has been shown to cause shrinkage of the new vessels in some patients, but the duration of effect is usually only for a month. Pan- retinal laser treatment provides better long-term control.
Severe proliferative diabetic retinopathy
In some patients, either without photocoagulation or if the photocoagulation and injections do not halt the disease, there can be progression to retinal detachment and vitreous hemorrhage. In those cases, vitrectomy surgery may be required to remove the blood and reattach the retina.
Macular Edema
Swelling of the macula is the most common cause of visual loss in diabetics. It can occur in any stage of retinopathy but is more common in the more advanced stages of the disease. It can be treated with laser photocoagulation and ocular injections. In patients with macular edema, both OCT testing and fluorescein angiography are usually necessary to identify the location and extent of the leakage.
Treatments
Intravitreal (Intraocular) Injections, Lucentis (ranibizumab, Genentech) and Eylea (aflibercept, Regeneron) have been demonstrated to produce the best visual acuity outcomes for macular edema and are first line therapies. Approximately 40% of diabetic patients receiving these injections had significant visual improvement of 3 lines of the visual acuity testing chart (compared to 15% with only laser), and 57% of patients had vision of 20/40 of better, which is required for driving (compared to 36% with only laser). This treatment is very effective, but often has to be repeated multiple times to reverse and stabilize macular edema. These drugs are antibodies to vascular endothelial growth factor (VEGF). VEGF is produced in diabetic eyes and makes the retinal blood vessels leaky (resulting in macular edema) and may also cause abnormal blood vessels to grow (resulting in proliferative retinopathy, bleeding, and retinal detachment). Lucentis and Eylea bind to VEGF and block its effects and may actually reduce the degree of diabetic retinopathy minimizing need for future laser treatments.
Vabysmo (faricimab, Genentech) is a more recent medication FDA approved for the treatment of diabetic macular edema and diabetic retinopathy. Vabysmo is an antibody that acts against both VEGF and Angiopoietin-2 (Ang-2). Some patients may require less frequent injections with Vabysmo. Almost 80% of patients in the clinical trial were able to be extended up to a 3-month interval at 2 years of treatment.
Another similar anti-VEGF drug, Avastin (bevacizumab, Genentech), is sometimes used when insurance does not cover Lucentis. This drug is also effective, but it is “off-label” (not FDA-approved for use in the eye) and has the risks of coming from a compounding pharmacy, as opposed to directly from the pharmaceutical manufacturer.
Finally, in some cases steroids (Kenalog, Triessence, Ozurdex, and Iluvien) may be used. They may be effective as additional therapy when laser and anti-VEGF drugs are not sufficient, do not produce a response, or a longer effect is desired. They act by reducing inflammation that may produce macular edema from leaky retinal blood vessels. We typically use steroids in con- junction with anti-VEGF agents rather than as first-line treatment as there are some risks of increasing cataract development or increase in intraocular pressure (glaucoma).
Surgical device implantation
Susvimo (ranibizumab, Genentech) is a port delivery system that is surgically implanted and is recently FDA approved for the treatment of diabetic macular edema and diabetic retinopathy. The implant allows sustained release of ranibizumab. Patients typically receive an in-office refill of the surgical implant every 6 months. This surgical procedure helps limit the number of injections patients need and may be a suitable option for some patients.
Pan-Retinal Laser Photocoagulation
Proliferative diabetic retinopathy, the most severe form of retinopathy is treated by a different form of laser treatment called pan-retinal photocoagulation. This form of laser has been shown to reduce the risk and rate of blindness by fifty percent in all stages of pre-proliferative and proliferative retinopathy. This treatment can be performed in the office over several sessions. This treatment was the ‘gold-standard’ for 40 years but now may be able to be deferred in patients who show good regression of disease with anti-VEGF injections.
Vitrectomy
If laser treatment or injection is unsuccessful, or if treatment is delayed, more advanced complications like vitreous hemorrhage or retinal detachment may develop. Vitreous hemorrhage may clear spontaneously or may be treated by a surgical procedure called vitrectomy. In vitrectomy, special instruments are used to go into the eye to remove the blood and scar tissue so that the center of the eye is clear for light to pass through and to remove the tractional forces which detach and distort the retina. Vitrectomy surgery is performed in the hospital operating room as an outpatient procedure. Often, additional laser photocoagulation is added at the time of vitrectomy surgery.
What is a cataract and should I have it removed?
A cataract is a clouding of the normal lens of the eye. While very common in the general population, cataracts develop earlier and more often in diabetics. Normally, cataracts can be easily treated by surgery to remove the cloudy lens and replace it with an artificial lens. The surgery has a high success rate, however, for patients with diabetes, the visual success rate is much lower. One reason for the poor vision is that diabetic retinopathy is present and goes undetected prior to the surgery. Even if there is no retinopathy prior to cataract surgery, the cataract extraction may cause macular edema.
Many diabetic patients have uncomplicated cataract surgery, but do not have visual improvement because the surgery causes swelling in the macula. This special problem does not mean that diabetic patients should not have cataract surgery, but diabetic patients should be carefully evaluated prior to any surgery. Significant diabetic retinopathy should be treated prior to the cataract surgery.
What is neovascular (rubeotic) glaucoma and why does it occur in diabetic patients?
In patients with advanced ischemia in the eye, neovascularization develops. This means that new blood vessels are growing along the surface of the retina or in front of the eye on the iris and in the trabecular meshwork. In the back of the eye, hemorrhage and retinal detachment may develop. In the front of the eye, these new vessels block the drainage mechanism of the eye and fluid cannot get out of the eye. Since the wall of the eye is rigid and cannot expand, the pres- sure in the eye becomes elevated. In eyes with elevated pressure, damage to the optic nerve occurs, which can lead to blindness. In some patients there is an acute rise in pressure, causing corneal edema, which can be painful. Some patients with severely elevated intraocular pressures develop nausea, vomiting or pain. The increase pressure in rubeotic glaucoma is treated with medications to lower the pressure. The rubeosis has been shown to respond remarkably to injections with anti-VEGF drugs and also to pan-retinal laser photocoagulation. These treatments get the blood vessels to go away so that the drainage mechanism may work better. If drops, injections, and laser don’t control the glaucoma, then surgery may be necessary to make another drain so that the pressure in the eye is normalized.
What is optic neuropathy?
The optic nerve carries the electrical signals that the retina produces back to the brain where the impulses are interpreted. The optic nerve needs a blood supply in order to function properly. Just like the retina, the optic nerve can be affected by closure of the blood vessels and ischemia. There is no effective treatment at this time for diabetic ischemic optic neuropathy.
Can I take aspirin?
The optic nerve carries the electrical signals that the retina produces back to the brain where the impulses are interpreted. The optic nerve needs a blood supply in order to function properly. Just like the retina, the optic nerve can be affected by closure of the blood vessels and ischemia. There is no effective treatment at this time for diabetic ischemic optic neuropathy.
Will I go blind?
There is no reason for patients, who accept the diabetic lifestyle, follow their medical doctor’s instruction and seek appropriate ophthalmologic care, to lose their eye sight. It is essential, how- ever, to achieve good metabolic control and to see a retinal specialist at appropriate intervals.