Retinal Detachments
What is a retinal detachment?
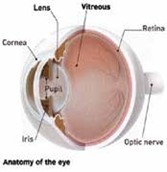
The retina is the light sensitive layer covering the inside of the back of the eye. It is analogous to the film in a cam- era. The retina has many layers. The rods and cones are in the layer that converts light to nerve impulses. The nerve impulses travel through the op- tic nerve to the brain where they are processed as vision. The bottom layer of the retina is the pigmented cell layer. Accumulation of fluid between the pigmented cell layer and the layer of rods and cones is called a retinal detachment. When retinal detachment is present, the fluid is called subretinal fluid and is in the sub-retinal space.

What causes retinal detachment?
There are three major types of retinal detachments. The most common type of retinal detachment is caused by a retinal hole or tear (which are both con- sidered retinal breaks) that allows fluid to pass from the central vitreous cavity of the eye into the subretinal space. This is referred to as a rhegmatogenous retinal detachment.
The second type of retinal detachment is caused by stretching and tenting of the retina by scar tissue in the vitreous cavity or scar tissue in the subretinal space. This is called a traction retinal detachment and is seen most commonly in advanced diabetic retinopathy and can be a component of recurrent rhegmatogenous detachment.
The third type of retinal detachment is caused by leakage of fluid into the sub- retinal space from the layer underneath the retina called the choroid. When this occurs without any retinal break present, the detachment is called an exudative detachment and is seen with tumors, inflammatory conditions, and other diseases of the layer underneath the retina called the choroid.
These pages will deal mainly with rhegmatogenous retinal detachments.
How do I know if I have a retinal detachment?
The symptoms of a retinal detachment depend on how far it has progressed. Some patients are completely unaware of any symptoms, in which case an eye doctor usually discovers the retinal detachment during an examination of the retina. Retinal tears that cause a rhegmatogenous retinal detachment may cause the patient to see flashing lights, which are usually much more noticeable in the dark. Bleeding from blood vessels broken during the retinal tear formation can cause floaters and smoky or hazy vision.
Retinal breaks usually occur in the peripheral retina that corresponds to your side vision. When the retinal detachment begins to spread from a retinal break, you may notice a dark curtain in your side vision. Unlike the transparent- curtain effect that floaters sometimes cause, the curtain seen with a retinal detachment has a solid appearance and usually will remain the same after moving the eye around by looking in various directions. The curtain can be seen in the side vision, in the up, down, right, left or diagonal positions and usually has a curved border or edge. As the detachment enlarges further, it can spread through the center of the retina called the macula. This results in loss of reading vision and straight-ahead vision.
As the detachment spreads further, the whole retina may detach, resulting in the patient only being able to detect the presence or absence of light or vague perceptions of motion. If a retinal detachment has been present for a year or more, the eye may no longer perceive light.

What should I do if I think I have a retinal detachment?
If you believe that you have a retinal detachment, you should find an eye doctor who is qualified to examine the retina for this diagnosis. The eye usually needs to be dilated with drops to allow an adequate examination of the peripheral retina where the retinal tears are usually located.
How will the doctor determine whether or not I have a retinal detachment?
The doctor will examine your retina and the other parts of the eye with a slit lamp (which is like a small microscope on a table top) and an ophthalmoscope. The indirect ophthalmoscope, which is worn on the doctor’s head, is combined with pressure on the eye (scleral depression). This will bring the peripheral retina, where the tears often are located, into view.
What will the doctor do if I just have a retinal break?
If you have flashers or the recent onset of floaters, the retinal break will usually be treated with laser or freeze treatment. Some retinal breaks are merely observed and are only treated if progression to retinal detachment occurs.
What will the doctor do next if I have a retinal detachment?
Usually a drawing of the retina is made showing the details of the retinal detachment. The doctor will then confirm whether you have a retinal detachment. The retinal drawing can be used to explain the size, location and cause of the retinal detachment to you. The doctor will then discuss the treatment options.
How are retinal detachments repaired?
Small numbers of detachments are merely observed for progression (worsening), but most require surgical repair. Depending on the size, location, duration, severity and type of the retinal detachment, the surgery may require laser (laserpexy) or freeze treatment (cryopexy) alone, pneumatic retinopexy, scleral buckling, vitrectomy with intraocular gas, vitrectomy with intraocular silicone oil or various combinations of these procedures.
How does the doctor decide which operation to do?
Deciding which surgery to do depends on the particular findings in a particular patient. There is controversy among retinal specialists about which surgery to do in certain situations. At Retina Associates of Florida, we try to balance risks and benefits for each patient’s situation in making these decisions. Our guiding principles in making the decisions are:
- Choose the least invasive surgery that has a reasonable chance of succeeding
- Do our best to save or restore vision
Factors that play into this decision include location and amount of retinal defects, whether previous cataract surgery has been performed, and patient ability to follow-up and comply with post operative instructions.

Observation
Observation is the least invasive and is usually reserved for very small detachments or for individuals that may not be candidates for any surgical procedure.
Laser Demarcation
Demarcation or walling-off the detachment with laser or freezing is the least invasive surgery. Although anesthetic injections to numb the eye may be given, no injections into the eyeball (intra- vitreal injections) are required. This surgery can usually be done in the doctor’s office. We treat about 5% of our patients with laser or freezing for demarcation.
Pneumatic Retinopexy
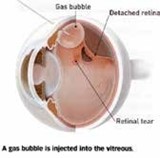
Pneumatic retinopexy is the next least invasive surgery. It utilizes a combination of laserpexy (sealing retinal tear with laser) or cryopexy (sealing the retinal tear with freezing treatment) and a gas bubble. After appropriate anesthetic injection, a gas bubble is injected into the vitreous cavity. The patient is then asked to position their head so that the bubble seals the retinal break.
The wall of the eye will then reabsorb the remaining subretinal fluid within a few days. Since the bubble reabsorbs after a week or more, cryopexy or laserpexy is applied around the retinal break to keep the detachment from coming back after the bubble reabsorbs. This procedure works best for recent detachments that do not have a retinal break in the bottom 1/3 of the retina. This procedure is usually done in our office. Success rates with this procedure are between 65-75%. Failures are usually due to new tears and can require additional surgery. Visual outcomes in patients who undergo subsequent retinal detachment repair after failed pneumatic retinopexy have been shown to be equivalent to those who undergo immediate vitrectomy or scleral buckling in the operating room.

Vitrectomy Surgery
Vitrectomy with intraocular gas is our most frequent choice if pneumatic retinopexy appears unlikely to work. Vitrectomy surgery is performed with small needle-sized cutting, illuminating, irrigating and grasping instruments inside the eyeball and is obviously more invasive. The surgery is viewed through the patient’s pupil with a microscope.
Near the end of the surgery the eye is almost always filled with air or gas. The surface tension holds the retina in place while the laserpexy or cryopexy placed around the retinal tears during the surgery creates a permanent seal of the retinal tears. The air or gas is reabsorbed by the body over time. With the newer surgical instrumentation and viewing systems, single surgery success approaches 90-92%. Recovery is usually quicker with less trauma and distortion to the eye than with a scleral buckle. Patients who haven’t previously undergone cataract surgery develop cataract more rapidly often requiring removal within the first 2 years after surgery.

Scleral Buckle Procedure
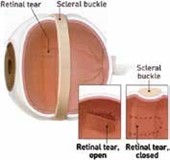
Scleral buckling was historically the main treatment for rhegmatogenous retinal detachment. It is done in the operating room with general or monitored anesthesia. A silicone rubber band or sponge is placed either under specific retinal breaks or in belt- like fashion around the whole peripheral retina, where existing breaks are located and where future tears might occur. Laser or cryopexy is placed around the tears to create a permanent seal. A small drainage incision is often made through the wall of the globe to remove subretinal fluid and to reattach the retina during the surgery. The scleral buckle elongates the eye, thereby making patients more near-sighted.
This can be troublesome to patients who have already had previous cataract surgery, and therefore is usually used secondarily in these patients if vitrectomy is unsuccessful. Single surgery success rates are around 82-85% when performed as the sole procedure.
Due to the modern development of pneumatic retinopexy and vitrectomy, we now treat only about 5% of patients with new retinal detachments with scleral buckling alone. We use it more commonly in patients that have their natural lens as the development of cataract change is lower than with vitrectomy.
Combined Vitrectomy / Scleral Buckle / Silicone Oil
Scleral buckling and vitrectomy with a gas bubble are frequently combined as the next surgery if pneumatic retinopexy or vitrectomy alone fails to reattach the retina on the first attempt. It is also used as an initial surgery if the detachment appears to be too difficult to repair by pneumatic retinopexy, vitrectomy, or scleral buckling alone. The procedure is usually performed in an outpatient operating room setting.
Vitrectomy with silicone oil is used for the more difficult retinal detachments. Some kinds of detachments requiring the use of silicone oil for a new detachment are giant tears, proliferative vitreoretinopathy (PVR, which is scar tissue formation on the retina and in the vitreous), young children and patients who need to fly home soon after surgery. The surgical technique and setting are the same as for vitrectomy with gas except that the surface tension of the silicone oil, instead of gas, is used at the end of the case. We treat less than 5% of patients with new retinal detachments with vitrectomy with silicone oil. The oil is usually removed in a separate procedure.
Where is the operation done?
Laserpexy and cryopexy are done at most of our office locations. Pneumatic retinopexy is done at a few offices. Scleral buckling and the vitrectomy procedures are done on an outpatient, day-surgery basis at a hospital or surgery center location.
What can I expect at the time of the procedure?
Laserpexy is done sitting at the slit lamp or lying down on a table, if the indirect delivery system is used. Topical drop anesthesia is always given, and a small injection of anesthetic may be given around the outside of the eyeball (periocular anesthetic injection) to numb it further.
Cryopexy is done with the patient laying back on a treatment table or a reclining chair. Periocular anesthetic injection is always required. The doctor will place a pen-size freeze probe on the outside of the eye and view the freeze application inside the eye with the indirect ophthalmoscope. The patient usually experiences a pressure sensation during the freeze application and some- times feels cold or mild discomfort.
Pneumatic retinopexy is frequently combined with cryopexy. The cryopexy is usually done first so that the eye is already anesthetized. After doing the cryopexy, the eye is usually painted with betadine solution to minimize the risk of infection. A small amount of fluid is removed from the front part of the eye (paracentesis) so that when a gas bubble is injected, the pressure won’t go too high. The gas bubble is then injected. The patient will usually be asked to roll over into the face down position for a few minutes after the gas bubble injection. The bubble can usually be seen as a dark disc or part of a disc that changes location with changes in head position. After reviewing instructions, the patient goes home.
The scleral buckling and vitrectomy procedures are done at the hospital or surgery center. This usually requires scheduling by our Surgical Coordinator, although sometimes it is scheduled on an emergency basis through the emergency room. The hospital has separate check-in and registration procedures and will inform you of the appropriate details.
What do I do after the operation?
After laserpexy or cryopexy delimitation, vigorous physical activity is usually restricted for about 2 weeks while adherence caused by the treatment reaches its maximum strength. This restriction applies to all of the more invasive procedures below.
After pneumatic retinopexy, you will be asked to position your head so that the gas bubble inside the eye is directly over the retinal breaks. You should not lie on your back because the bubble will not be in the right place and it may cause temporary glaucoma or cataract. Eye drops may be given for a few days to minimize the risk of infection.
After a scleral buckle, head positioning is not required unless a supplementary pneumatic retinopexy is done. You will be sent home from surgery the same day with an eye patch covering the operated eye.
Eye drops will usually be started the same day and tapered- off over 2 to 4 weeks. A follow-up appointment will be scheduled for you at our office, usually the next day. The eye patch and eye drops regimen, and follow-up appointment are the same for the vitrectomy procedures below.
After the vitrectomy procedures either by themselves or when combined with scleral buckling, head positioning is always required to place the gas bubble or silicone oil bubble where it is most effective and least likely to cause glaucoma or a cataract.
Can I fly in an airplane after the operation?
If you do not have a gas bubble, you can fly. If you do have a gas bubble in the eye, flying is not allowed because the bubble will expand rapidly in size at the reduced cabin air pressure. The high pressure caused by the expanding bubble will occlude the central artery and may even rupture the surgical wounds. This will lead to permanent blindness. The bubble will also expand if you receive nitrous oxide anesthesia. A medical alert bracelet will be placed on your wrist and should remain there until the bubble has completely absorbed. You are permitted to fly with silicone in the eye.
How long will it take to recover after the operation?
For laserpexy or cryopexy for delimitation, you return to work the next day for sedentary jobs but may be restricted from highly physically active jobs for up to 2 weeks.
After successful pneumatic retinopexy, most patients can return to sedentary jobs in about one week. You may be restricted for longer periods for more physically active jobs or if longer acting gas bubbles are used. Also, 30-35% of patients who have had pneumatic retinopexy will require further surgery thus extending their recovery.
For scleral buckling and the vitrectomy procedures, return to a sedentary job is often possible in about 2 weeks, but may take as long as 4 weeks if there is tearing, discomfort or an unusually red eye. For construction jobs and similar jobs with challenging work environments, return to work may delayed up to 2 months after surgery.
How much will I be able to see after the operation?
Recovery of visual acuity after retinal reattachment surgery is impossible to predict with certainty. The general rule is that the better your vision is before the surgery, the more likely you are to recover good vision after the surgery. In patients who have had detachment involving the macula (the center of vision) for a long time, good visual recovery is less likely. Patients who have PVR (scar tissue on the retina) are less likely to have good visual recovery and are also more likely to need a second operation to reattach the retina.
Patients with non-retinal eye problems, e.g., cataract, corneal cloudiness, glaucoma and optic neuropathy, are also less likely to have good visual recovery.
The primary goal of retinal reattachment surgery is to reattach the retina anatomically, since the patient will go blind in the eye if the retina is not reattached.
In most patients, vision that can be recovered will be recovered in 1 to 2 months. Further visual recovery can occur for up to 2 years after surgery. Specific problems such as macular edema, macular pucker, cataract, and corneal cloudiness can often be corrected with substantial further improvement of visual acuity.
What happens if the retina detaches again?
It is very important to persist in getting the retina reattached if the first attempt is not successful or even if the retina detaches again years later. If the retina is not reattached, eventually all vision will be lost in the affected eye.
If the previous surgery was not successful in maintaining retinal reattachment, a more invasive or more complicated procedure is chosen to counter the reasons the first operation was not successful. This is a common occurrence with pneumatic retinopexy in which the risk of having to have a second procedure is relatively high. The trade-off is that if the pneumatic retinopexy is successful, the recovery is faster, there is no need for operating room surgery and in some cases there is a better chance of getting back good vision.